Article en anglais
IAS 2017 – Paris
Sunday, 23 July 2017 – 14:45 -16:45
Venue: Room 241, Palais des congrès
Organiser :
Sidaction, founded in 1994, is a French NGO that raises awareness and funds biomedical and social science research projects, supports programs in prevention as well as ways to assist people affected by HIV. In France, Sidaction is the only AIDS non-profit organization funding research. Here, it gathers funded experts to discuss and debate the current state of the art.
Satellite title : Role of mucosa and myeloid cells in HIV pathogenesis
Description :
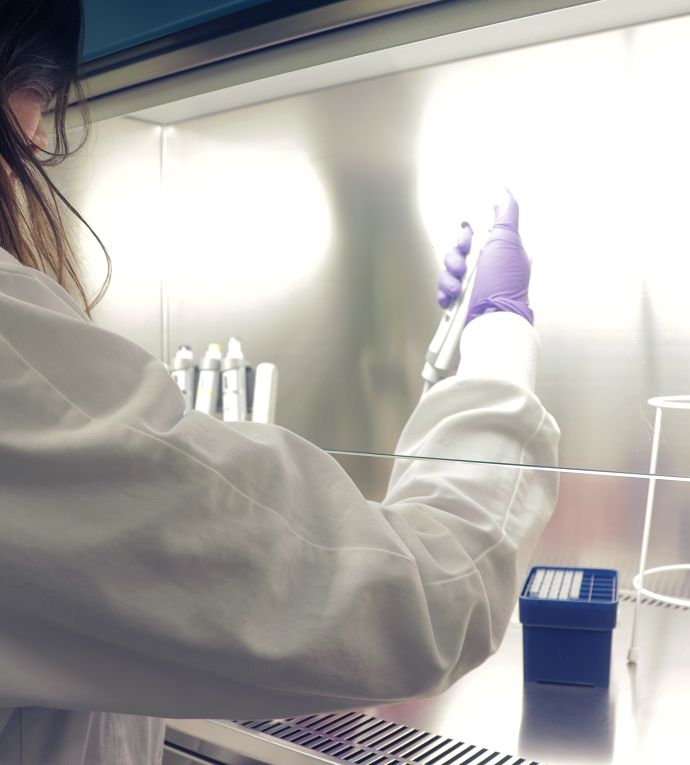
Genital and rectal mucosa are the primary site of entry and defense upon exposure to HIV. How the mucosa environment, including immune cells, influences HIV acquisition and persistence is of great importance. Myeloid cells are the first targets of infection and vehicles of viral dissemination, but they also orchestrate the primary intrinsic, innate and adaptive responses. Much still needs to be understood about this dual role.
Here, experts in the field will discuss the current state of the art on the role of mucosal tissue and its myeloid cells in HIV pathogenesis. Recent knowledge on the role of macrophages and dendritic cells as targets of infection and agents of anti-viral defenses will be presented. The role of mucosal immune responses, the influence of early treatment and the potential of mucosal vaccine strategies will be discussed. The influence of gender in the activation of innate immune responses will also be debated.
Chairs :
Jason Brenchley -Laboratory of parasitic diseases, NIAID, NIH
Dr. Brenchley received a master’s degree from Idaho State University in 1999 and received a Ph.D. from the University of Texas Southwestern Medical Center at Dallas in 2003. He joined NIH as a research fellow, studying immunopathogenesis and mucosal immunology in HIV-infected individuals. He has been a principal investigator at NIAID, NIH, USA since 2008. His work has, predominantly, focused on how immunological abnormalities within the GI tracts of HIV-infected individuals relates to microbial translocation, alterations to the microbiome, and systemic inflammation. He uses this knowledge to guide novel adjunctive therapeutic interventions.
Pierre Delobel -Centre de physiopathologie de Toulouse-Purpan, Toulouse
Pr. Delobel, MD, PhD is a Professor of Infectious Diseases and Head of Department at Toulouse University Hospital, involved both in clinical care and translational research on HIV infection.
He received his Ph.D. in Immuno-Virology in 2007 from Françoise Barré-Sinoussi’s laboratory at Pasteur Institute in Paris. His thesis work was on the influence of HIV-1 coreceptor usage on CD4+ T cell restoration under antiretroviral therapy. His current work focuses the mechanisms of poor immune reconstitution in the intestinal mucosa of HIV-infected subjects despite effective antiretroviral therapy, notably the chemokine networks driving T cell homing to the gut.
Speakers :
MODULATION OF CELL FREE AND CELL ASSOCIATED INFECTION BY HUMAN SEMINAL PLASMA IN THE COLON
Nathalie Dejucq – Rainsford – Institut de recherche en Santé, environnement et travail, Rennes
Nathalie Dejucq-Rainsford is a research director at the French National Institute of Health and Medical Research (INSERM). She heads a team of 30, studying the physiology and physiopathology of the uro-genital tract within the IRSET-INSERM U1085 in Rennes (France)(www.irset.org). Her research interest is at the interface between the biology of reproduction and virology/immunology. One specific aim of her research is to better understand viruses’ sexual transmission and the host local antiviral responses, with a focus on the male genital tract. In this respect, she has demonstrated that several semen-producing organs are infected by HIV/SIV in both humans and macaques, shown that male genital organs can constitute viral reservoirs and characterized the testicular antiviral defense system. She serves as an expert in several national and international committees.
Current work Summary : HIV colo-rectal transmission can be mediated by either free viral particles or infected cells in semen. Regarding cell free infection, we found that seminal plasma (SP) from HIV+ men is significantly less enhancing of HIV infection of CD4+T cells than SP from healthy donors, because of elevated concentrations of the CCR5 ligand RANTES in HIV+ SP (Camus et al, AIDS 2016). Regarding cell-associated infection, we observed a rapid transmigration of both T lymphocytes and macrophages across the intact epithelial barrier of polarized colon explants. This transmigration was also observed in the presence of SP, which did not modify the barrier permeability.
IgA TAGETING HIV-1 ENVELOPE gp41 TRIGGERS ANTIBODY-DEPENDENT CELL CYTOTOXICITY (ADCC) CROSS-CLADE, IN A PROCESS SYNERGIZED BY ANTI-HIV ENVELOPE IgG
Morgane Bomsel -Cochin Institute, Paris
Morgane Bomsel is research Director at CNRS and leads a team at Cochin Institute, Paris, France. Her lab is focused on deciphering the initial step of sexual transmission of HIV in the female and male genital tract and how the mucosal immune system can block the early step of infection. To elaborate a HIV preventive vaccine active mucosally, Morgane Bomsel’s lab focused on highly exposed but seronegative individuals, uninfected despite unprotected sex with HIV+ partners (ESN) and showed that ESN develop mucosal IgA with antiviral activities as correlate of protection. Epitopes of ESN IgA served as a basis for an HIV-1 vaccine design that when tested in monkey, fully protected animal from repeated vaginal infection. The vaccine was then successfully tested in a phase I clinical trial.
Current work Summary : To elaborate a prophylactic vaccine active mucosally against HIV a robust local IgA as well as IgG response against HIV-1 envelope gp120 or gp41 is highly desirable. In addition to broad neutralizing activity preventing infection, these antibodies should engage also the innate immune system to destroy early infected cells by antibody dependent cell cytotoxicity (ADCC). We now report for the first time that anti-gp41IgA lyse HIV-1 infected cell cross -clade by ADCC. Furthermore, anti- gp41 IgA and IgG cooperate to synergize ADCC. Thus, inducing mucosal IgA and IgG by vaccination will strength protection by complementary and synergistic activities with IgG.
Authors : Daniela Tudor1,2,3, Maxence Duchemin1,2,3, Marwa Khamassi1,2,3, Lin Xu1,2,3, and Morgane Bomsel1,2,3
1Laboratory of Mucosal Entry of HIV-1 and Mucosal Immunity, Department of Infection, Immunity and Inflammation, Cochin Institute, CNRS UMR 8104, Paris, France; 2INSERM U1016, Paris, France; 3Université Paris Descartes, Sorbonne Paris Cité, Paris, France
EARLY cART INITIATION PRESERVES GUT TFH AND GP140 SPECIFIC MEMORY B CELLS IN HIB-1 INDIVIDUALS
Sophie Hüe – Vaccine Research Institute, Créteil
Sophie HUE, MD, PhD is PU-PH (Professeur Universitaire-Praticien hospitalier) at the East Paris University (UPEC), France. She obtained her PhD from Paris V University (France) following her work on the role of NKG2D/MICA interaction in villous atrophy during coeliac disease. She then moved to Oxford University to perform her postdoctoral trainee in the lab headed by Fiona Powrie, where she studied the role of IL23 in inflammatory bowel disease.
Since 2007, she works in the team 16, INSERM U955, part of the Labex Vaccine Research Institute (VRI). Her research is focused on the interaction between the commensal flora and the immune system in the gut. Today, her work is focused on B cell responses in the gut of HIV infected patients. These studies are performed with the ultimate aim to provide novel insights for research on therapeutic and preventive vaccines.
Current work Summary : In this study, we asked the question whether the timing of cART initiation may have an impact on the development of the HIV-1-specific humoral immune response in the gut. We found that early treatment was associated with an increased frequency of functional intestinal resting-memory B cells. The frequency of resting memory B cells strongly correlated with the frequency of follicular helper T (TFH) cells in the gut. Importantly, the frequency of HIV-1 Env gp140-reactive B cells was higher in e-ART patients and we found an increased production of gp140-reactive IgGs by mucosal B cells after stimulation in e-ART patients. Our results demonstrated that early initiation of cART helps to maintain HIV-1-reactive memory B cells in the gut as well as TFH cells that are of utmost importance for the development of potent affinity-matured and broadly neutralizing antibodies.
SENSING OF HIV-1 ENTRY TRIGGERS A TYPE I INTERFERON RESPONSE IN HUMAN PRIMARY MACROPHAGES
Philippe Benaroch– Curie Institute, Paris
Philippe Benaroch is expert in protein intracellular trafficking in immune cells. He is very interested in cell biological aspects of the relationship between immune cells and viruses. After a Ph. D. in Immunology at the Institut Pasteur, he spent two years at the MGH-Harvard University and at the MIT (Boston, USA), as a post-doctoral fellow in immunobiology. He is best known for his contribution on MHC class II intracellular trafficking and on the HIV cycle in primary macrophages. For the last 10 years, Philippe Benaroch has led a group at INSERM U932 Institut Curie. His team is now focused on two main topics; the detection of the viral infection at the endosomal level by the innate immune system and the HIV cycle in primary immune phagocytes.
Current work Summary : HIV-1-infected macrophages are found in many tissues of infected patients even under anti-retroviral therapy and are considered a viral reservoir. How HIV-1 is detected and what type of responses are elicited upon sensing remain in great part elusive. Our study provides evidence that macrophages can detect HIV-1 as soon as it enters the cell before retro-transcription takes place. This sensing triggers a low interferon response, which activates an anti-viral program protecting cells against further viral challenge and thus potentially limiting the spread of the infection.
Authors : Jérémie Decalf 1*, Marion Desdouits1*, Vasco Rodrigues1, François-Xavier Gobert1, Matteo Gentili1, Santy Marques-Ladeira1, Célia Chamontin2, Marylène Mougel2, Bruna Cunha de Alencar1,3, Philippe Benaroch1#
1Institut Curie, PSL Research University, INSERM U932, Paris, France ; 2Institut d’Infectiologie de Montpellier, CNRS UMR9004, Montpellier University, France ; 3 Instituto de Ciências Biomédicas, Universidade de São Paulo, Brazil
* JD and MD contributed equally to this work
INTERFERON-INDUCED TRANSMEMBRANE PROTEINS (IFITMs) AND THEIR ROLE IN THE RESTRICTION OF HIV-1 REPLICATION
Andréa Cimarelli – International Center for Infectiology Research (CIRI), Lyon
Andrea Cimarelli obtained his PhD at the University of Pavia, Italy, in 1996. He then performed his postdoctoral training at Columbia University, New York, in the laboratory of Dr. J. Luban, where he studied the mechanism underlying the assembly of virion particles of HIV. In 2000 he joined the laboratory of Dr. J.L. Darlix at the Virology Unit of INSERM at the Ecole Normale Superièure de Lyon and from 2005 he directs a group of research focused on the study of human lentiviruses. Starting 2013 the laboratory joined the International Center of Research in Infectiology (CIRI) of Lyon affiliated to the ENS-LYON.Andrea Cimarelli is currently head of the lentiviral infection laboratory, delegate director of the CIRI and member of the scientific commission 1 of the ANRS.
Current work Summary : IFITMs are innate defense proteins that inhibit a broad range of viruses. For HIV, IFITMs have been associated to two distinct mechanisms of inhibition: endosomal sequestration of incoming virions in target cells; interference with the infectivity of newly-produced virions However, the molecular mechanisms at play remain unknown.
Using IFITM3 as a paradigm for the IFITM family, we have identified multiple domains required for the negative imprinting of HIV-1 virions gathering important molecular insights into their action against HIV. These and other results on the characterization of the action of IFITM3 on the negative imprinting of HIV-1 virions will be presented.
Authors : Romain Appourchaux1-5,Kevin Tartour1-5, Julien Gaillard6, Xuan-Nhi Nguyen1-5, George Savidis7, Abraham Brass7, Philippe Roingeard6, 8and Andrea Cimarelli1-5*
1 CIRI, Centre International de Recherche en Infectiologie, Lyon,F69364, France ; 2 INSERM, U1111, 46 Allée d’Italie, Lyon, F69364, France ; 3Ecole Normale Supérieure de Lyon, 46 Allée d’Italie, Lyon, F69364, France ; 4 CNRS, UMR5308, 46 Allée d’Italie, Lyon, F69364, France ; 5 University of Lyon, Lyon I, UMS3444/US8 BioSciences Gerland, Lyon, F69364, France ; 6 Plateforme des Microscopies, PPF ASB, Université F. Rabelais et CHRU de Tours, 37032 Tours, France ; 7Department of Microbiology and Physiological Systems, University of Massachusetts Medical School, Worcester, MA 01655, USA ; 8 INSERM U966, Université F. Rabelais et CHRU de Tours, 37032 Tours, France
SINGLE CODON-MEDIATED CONTROL OF TLR7 PROTEIN DOSAGE AFFECTS TYPE I IFN-PRODUCTION BY PLASMACYTOID DENDRITICS CELLS IN A SEX SPECIFIC MANNER
Jean-Charles Guéry– Centre de physiopathologie de Toulouse-Purpan, Toulouse
Jean-Charles Guéry is research Director of INSERM and leads a team at CPTP interested in understanding the mechanisms by which sex specific factors regulate the immune responses in preclinical models of human diseases (CNS autoimmunity, allergic diseases), as well as through the analysis of the impact of sex-dependent factors on human immune cell phenotype and functional properties in the context of systemic lupus erythematous and HIV-1 infection. His research strategy favors « bedside to bench » approaches, which he believes are more promising with respect to clinical relevance.
Current work Summary : Men and women differ in their susceptibility to HIV-1 infection and disease progression. Plasmacytoid dendritic cells (pDCs) promote antiviral immune responses and contribute to the early production of type I IFNs through TLR7 activation by HIV-1 RNA. Here we uncovered a role for a frequent SNP of TLR7 as a determinant of defective TLR7-driven production of type I IFNs by pDCs in women, but not in men, in line with a sex-specific effect on HIV-1 acquisition.
Authors : Pascal Azar1,2, José Enrique Méjia1,2, Claire Cénac1,2, Mary Requena1,3, Michelle Cazabat1,3, Romain Carcénac1,3, Jacques Izopet1,2,3, Pierre Delobel1,2,3 and Jean-Charles Guéry1,2,*.
1Centre de Physiopathologie de Toulouse Purpan, INSERM UMR1043, CNRS UMR5282, Toulouse, France ; 2Université Paul Sabatier, Toulouse, France ;3Laboratoire de Virologie, CHU Purpan, Toulouse, France.
 Session satellite IAS 2017 : Le rôle des muqueuses et des cellules myéloïdes dans la pathogenèse du VIH
Session satellite IAS 2017 : Le rôle des muqueuses et des cellules myéloïdes dans la pathogenèse du VIH